Ticks and Disease in Kentucky
ENTFACT-618: Ticks and Disease in Kentucky | Download PDF | En Español
by Anna Pasternak and Jonathan Larson (University of Kentucky Entomology) and Monica Cipriani (University of Kentucky Epidemiology)
University of Kentucky College of Agriculture

A tick questing on the end of a leaf. The front legs are outstretched to find and grab onto a host.
What Are Ticks and Why Are They Important?
Ticks are hemimetabolous, meaning they go through incomplete metamorphism. In the entomology world, this means their lifecycle consists of 4 life stages: egg, larva, nymph and adult. When larvae hatch from the egg they are very tiny—smaller than 2mm in size! The larva will find a host—usually a small mammal—and feed for ~2-3 days, then molt into a nymph. The nymph will feed again, this time for ~4-7 days, then molt into an adult. Adult females will take a final bloodmeal for ~7-10 days, mate with a male, lay eggs, and die. Adult males can bite but they do not engorge themselves. Most ticks will feed on three separate hosts in their lifetime—these are called three-host ticks. Two-host ticks stay and feed on the same host in the larval and nymphal stage, then drop off to find a different host as an adult. One-host ticks remain and feed on the same host during their whole life.
There are over 700 species of ticks worldwide. All of them are grouped into one of the three families: Ixodidae (hard ticks), Argasidae (soft ticks), and Nuttalliellidae. Nuttalliellidae consists of one species, Nuttalliella namaqua, and is native to Africa. Argasidae ticks are soft bodied and are usually found hiding in caves and burrows. Neither of these species are commonly encountered by humans. When most people think about ticks, they’re thinking of Ixodidae. Most tick species fall into this family and are called “hard ticks” because they have a scutum that acts like hard, protective shield on their dorsal (back) side. On adult females, the scutum only comes about halfway down the body while in males it covers the whole dorsal side, making differentiating between male and female adults easy. The body of a tick is composed of the alloscutum, which engorges and fills with blood as the tick feeds, the scutum, and the capitulum which makes up the mouthparts. The mouthparts include the basis capitulum that attaches to the palps and hypostome. Palps protect the hypostome, which is what is inserted into the host and sucks up blood like a straw. Chelicerae help cut through the skin and make a small pool of blood underneath the skin’s surface for the tick to drink from. Small hooks on the hypostome, called denticles, anchor the hypostome in place. The saliva of ticks plays a major role in blood feeding. The saliva contains things like anticoagulant and anti-inflammatory molecules that suppress host immune systems and allow the tick to go unnoticed while feeding.

A female (left) and male (right) Blacklegged tick. Notice how the scutum on the female only comes halfway down the body.
Ticks can be important vectors of disease. Sometimes, when a tick feeds on a host it will pass along pathogens that can cause disease such as bacteria, viruses, and protozoa. You’ve probably heard of some of these tick-borne illnesses, like Lyme disease or Rocky Mountain Spotted Fever or even people becoming allergic to red meat after a tick bite. Ticks will pick up these pathogens from “natural reservoirs” which are organisms or a specific environment in which an infectious pathogen naturally lives and reproduces. A common natural reservoir for the bacteria causing Lyme disease are white-footed mice.
Not all tick species can vector every pathogen, and not every tick bite results in disease. For example, being bitten by a Lone Star tick poses no threat of developing Lyme disease because this tick species cannot carry or vector the pathogen. Now, let’s say that you find a Blacklegged tick attached to you or someone else. This tick can carry and vector the bacteria that causes Lyme disease, but the tick must feed for a long time—about 36 hours—before the bacteria is transmitted into the host. Different pathogens take different amounts of time to be transmitted. Some pathogens, however, can be transmitted almost immediately once a tick bites, which is why prevention of ticks is an important precautionary step that everyone should take.
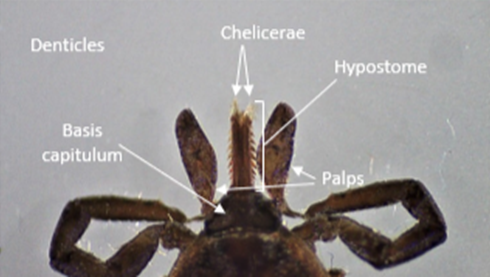
The mouthparts of a tick, also known as capitulum.
Ticks in Kentucky
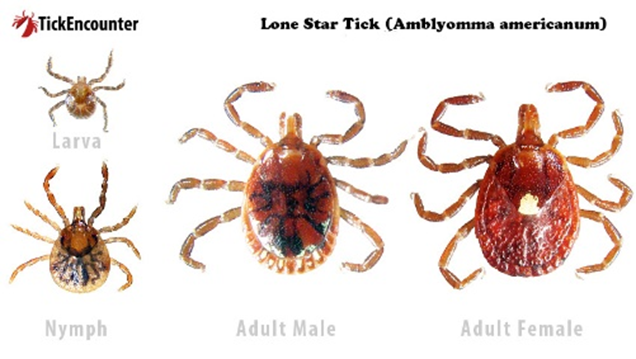
Lone Star tick (Amblyomma americanum)
Seasonality: Adults and nymphs active March through September, with larvae active in the later summer and fall months.
Habitat: Can be found in woodland and forest areas, and open areas with dense vegetation.
Identification: Reddish brown body color with a triangular scutum on adult females. Adult females also have one white dot on their dorsal side. Adult males have smaller white markings along the posterior end of the dorsal side at the end of their scutum. Mouthparts are long. Nymphs and larvae are reddish brown and have a circular body shape.
Diseases: Bourbon virus, Ehrlichiosis*, Heartland virus, red meat allergy*, Rocky Mountain Spotted fever*, Southern tick-associated rash illness (STARI), Tularemia*.
Fun facts: Lone star ticks are active questers meaning they will chase their host. This species is very common in Kentucky and is often present in large numbers.
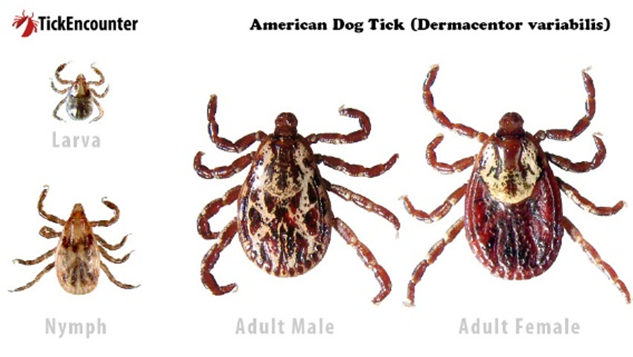
American Dog Tick (Dermacentor variabilis)
Seasonality: Adults and nymphs active March through September. Nymphs and larval stages of this species are not commonly encountered by humans.
Habitat: Can be found along forest & trail edges, as well as in fields and meadows.
Identification: Brown body with an oval-shaped scutum on adult females. Adults have a complex white pattern on the scutum and short mouthparts. Nymphs and larvae are brown or tan.
Diseases: Rocky Mountain Spotted fever* and Tularemia*.
Fun facts: Adult American dog ticks can survive for up to two years without feeding.
Blacklegged Tick (Ixodes scapularis)
Seasonality: Year round with adults active October-June and nymphs active May-August.
Habitat: Woodland and forested areas that have dense leaf litter on the ground floor.
Identification: Adults have a reddish-orange body with black legs and scutum. Nymphs and larvae have a translucent body with black scutum and legs. Mouthparts are long.
Diseases: Anaplasmosis*, Babesiosis, Lyme disease*, Powassan virus, and Relapsing fever.
Fun facts: Only ticks that belong to the genus Ixodes can transmit the pathogen causing Lyme disease. While most ticks undergo diapause during the winter month, blacklegged tick adults remain active when temperatures are above 40º F.

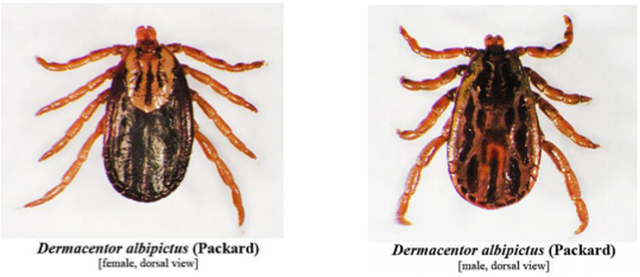
Winter Tick (Dermacentor albopictus)
Seasonality: Year-round but uncommonly encountered by humans as this species spends its whole life on one host. Seasonality in Kentucky is still under investigation.
Habitat: Woodland and forested areas.
Identification: Brown body with complex pattern similar to the American Dog tick, but the patterns are paler in color. Mouthparts short.
Diseases: No diseases of medical concern.
Fun facts: Winter ticks are a 1 host species of tick. They are sometimes called the “moose tick” as they tend to parasitize moose. While they are not important vectors of disease, they can cause major hair loss on hosts.
Winter Tick (Dermacentor albipictus) Female (left) and Male (right)
Asian Longhorned Tick (Haemaphysalis longicornis)
Seasonality: Seasonality in Kentucky is still under investigation. In other eastern states, it seems to be active March-September.
Habitat: Woodland areas and fields.
Identification: Brown bodies with no identifiable markings. Mouthparts are short.
Diseases: Possible vector of Theileria orientalis.
Fun facts: This species is the first known invasive tick species in the United States. It is parthenogenic, meaning that females do not need to mate to reproduce.

Brown Dog Tick (Rhipicephalus sanguineus)
Seasonality: Seasonality in Kentucky is still under investigation. In other states, it seems to be active year-round.
Identification: Brown body in a teardrop shape. Mouthparts are short.
Diseases: canine babesiosis, canine ehrlichiosis, Rocky Mountain Spotted fever*.
Fun facts: This species, unlike other ticks, can survive its entire life indoors. Its preferred host is the domesticated dog and will likely enter your home by hitch-hiking on your furry friend.

Gulf Coast Tick (Amblyomma maculatum)
Seasonality: Seasonality in Kentucky is still under investigation. In other states, it seems to be active March-November.
Identification: Brown body and legs with a white complex pattern. Mouthparts are long.
Diseases: R. parkeri, a form of spotted fever.
Fun facts: As the name implies, this tick prefers coastal grasslands for habitat. In Kentucky, they can be found in areas of tall grass and meadows.

Gulf Coast Tick Female (left) and Male (right)
Protecting Yourself, Others, and Pets
Significant increases in wildlife populations, expanded ranges of some tick species, development of housing in rural areas, and the popularity of hiking and ecotourism have increased the potential for people to encounter ticks. Awareness and use of preventive measures to reduce exposure while working outdoors or enjoying outdoor activities are keys to reducing tick bites. Use repellents and check yourself frequently for ticks while and after being in areas where they may be active.
The best strategy to reduce the potential of contracting tick-borne diseases is to avoid tick bites. Here are some tips:
- Avoid walking through uncut fields, brush and other areas likely to harbor ticks. Walk in the center of mowed trails to avoid brushing up against vegetation.
- Use a repellent that contains 20 to 30 percent DEET on exposed skin. Always follow product instructions.
- Use products that contain permethrin to treat clothing and gear, such as boots, pants (especially the cuffs), socks and tents.
- Tuck long pants into your socks and boots. Wearing light-colored pants makes ticks easier to see.
- In areas where there are ticks, check yourself, children and other family members for ticks every 2 to 3 hours and upon returning home from hikes and outdoor activities. Examine behind ears, hair, neck, legs and around the waist.
- If you let your pets outdoors, check them often for ticks. Ticks can “hitch a ride” on your pets, but fall off in your home before they feed. Tick collars, sprays, shampoos, or monthly “top spot” medications help protect against ticks.
How to Remove a Tick Safely
Step 1: Use fine-tipped tweezers to grasp the tick as close to the skin's surface as possible. the goal is to remove the entire tick including its head and mouth.
Step 2: Pull up with steady, even pressure. do not twist or jerk the tick.
Step 3: Clean the bite area and your hands with rubbing alcohol, an iodine soap, or soap and water.
A feeding tick holds itself in place by barbed mouthparts and a type of glue. Grasp it with fine-point tweezers as close to the skin as possible. Pull it straight out gently but firmly. Do not twist or jerk the tick during removal. Afterwards, wash the bite area and your hands thoroughly with soap and water and apply an antiseptic to the bite site.
You can store removed ticks in a sealed plastic bag with the date and location noted. Identification of ticks is available through your local Cooperative Extension Service office.
Anyone with concerns about exposure to ticks and possible disease transmission should consult their physician to determine the best course of action. Most tick-borne diseases can be averted by early intervention with an antibiotic.
Tick-Borne Diseases Reported in Kentucky
Rocky Mountain Spotted Fever (Spotted fever rickettsiosis)
Typical symptoms include fever, headache, abdominal pain, vomiting, and muscle pain. A rash also may develop. The rash is characterized by small, flat, pink, non-itchy spots that first appear on the wrists, forearms, and ankles and gradually spreads towards the trunk of the body.Rocky Mountain spotted fever can be a severe or even fatal illness if not treated in the first few days of symptom onset. Reservoir animals include deer mice, meadow voles, and other small mammals. Dogs are susceptible to infection but the disease is rarely diagnosed in cats.
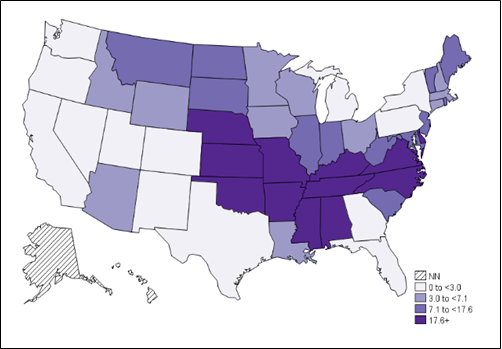
Annual incidence (per million persons) of Rocky Mountain Spotted Fever in the United States – 2018.
Erhlichiosis
This results from infection by one of several species of bacteria. Flu-like symptoms such as mild muscle aches, fatigue, and occasionally severe fever appear within 1 to 2 weeks after a bite by an infected tick. A rash may also develop, most commonly in children, and appear as flat, red, discolored dots. Ticks appear to have to feed for about 24 hours before disease transmission occurs. White-tailed deer, elk, and wild rodents are reservoirs of the disease.
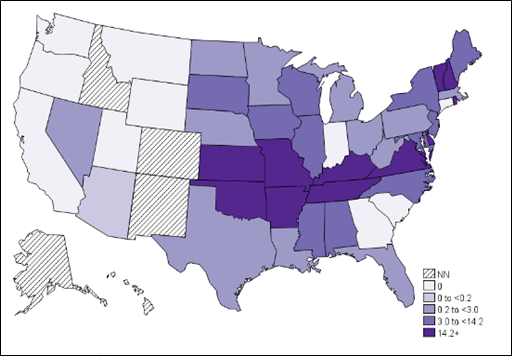
Annual incidence (per million persons) of Ehrlichiosis in the United States – 2018.
Lyme Disease
Caused by a bacterium transmitted by the bite of infected blacklegged ticks. In most cases, the tick must be attached for several hours before transmission occurs. A characteristic bulls-eye rash may accompany the typical flu-like symptoms in early stages of infection. If not treated, Lyme disease can spread to the heart, nervous system, and joints. In some cases, after treatment, persons can continue experiencing symptoms through a condition called Post-Treatment Lyme Disease Syndrome (PTLDS). White-footed mice are an important reservoir of the disease.
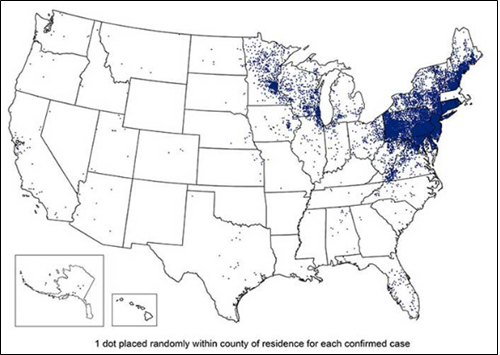
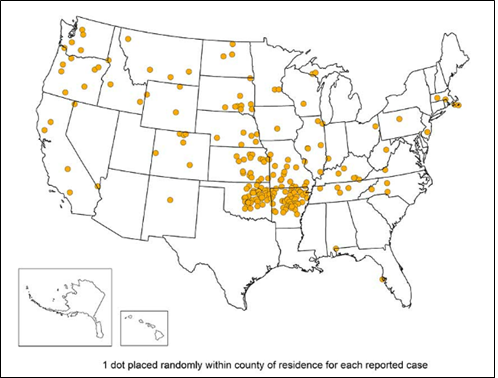
Reported cases of Lyme disease in the United States – 2018.
Anaplasmosis
A bacteria disease that was recognized in humans in the mid-1990’s. Symptoms are usually mild flu-like symptoms in the early stages of infection that often develop 1 to 2 weeks after being feed upon by an infected tick. If left untreated, symptoms may progress to late stage illness and become more severe and dangerous. White-footed mice, short-tailed shrews, and eastern chipmunks are among the reservoir hosts of this disease.
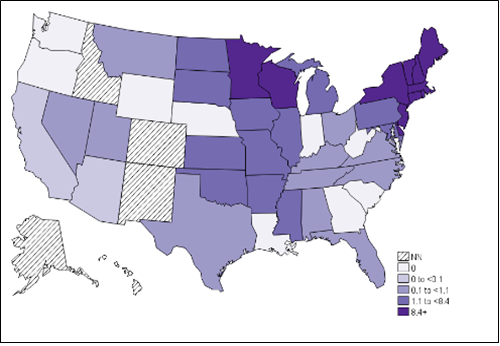
Annual incidence (per million persons) of Ehrlichiosis in the United States – 2018.
Tularemia
This illness can be spread to humans several different ways, including by the bite of an infected tick. It is a rare but potentially fatal bacterial disease of rabbits, hares, and rodents; however, it can infect more than 100 species of wild and domestic animals. American dog ticks an d lone star ticks can transmit the disease to humans. In addition, humans can contract tularemia when handling infected animals. Signs and symptoms vary with the method of entry into a person but a fever accompanies all forms. Cats and dogs may contract the disease by eating flesh of infected animals or through tick bites.
Reported cases of Tularemia in the United States – 2018.
Red-Meat Allergy
This may appear as a skin rash or anaphylactic reaction that occurs 3 to 6 hours after eating beef, pork, or lamb. The reaction can occur in people with a history of strong reactions to tick bites (redness and itching at bite sites that last for weeks) or many bites from a single incidence. They produce antibodies to proteins in the saliva of feeding lone star ticks. The common sugar (alpha-gal) that causes the reaction is not present in chicken, turkey, or fish. This antibody has been found in up to 20% of people tested who live where the lone star tick is common.
References
Kentucky Department of Health: Tickborne Diseases
Revised: 6/2021
CAUTION! Pesticide recommendations in this publication are registered for use in Kentucky, USA ONLY! The use of some products may not be legal in your state or country. Please check with your local county agent or regulatory official before using any pesticide mentioned in this publication.
Of course, ALWAYS READ AND FOLLOW LABEL DIRECTIONS FOR SAFE USE OF ANY PESTICIDE!